PUBLISHED: 21st October 2024

This year, FORCE conducted surveys for people at increased risk for hereditary cancers. Results from our first segment, for people at high risk for breast cancer, highlight the need for continued outreach, partnerships and programs focused on the hereditary cancer community.
FORCE (facingourrisk.org) is a national nonprofit organization focused on helping people and families affected by inherited cancer risk. Our community is comprised of people with inherited mutations in genes linked to cancer, including BRCA1, BRCA2, ATM, BRIP1, CDH1, CHEK2, PALB2, PTEN, RAD51C, RAD51D, TP53 and the Lynch syndrome genes, EPCAM, MLH1, MSH2, MSH6 and PMS2.
The burden of hereditary cancers
Cancer takes an enormous toll on the person diagnosed, as well as their friends, relatives and caregivers. This is amplified for people with hereditary cancer risk. Inherited mutations tend to cause:
- Younger onset cancers, often during childbearing years.
- Risks for multiple primary cancer diagnoses.
- Risks that run in families and are shared with blood relatives.
About the survey and respondents
People at increased risk for breast and gynecologic cancer were invited to complete our survey from 02/12/2024 to 5/14/2024. The survey data included responses from 1,261 people.
More than half of the respondents had a BRCA1 (26%) or BRCA2 (32%) mutation. The next most common mutations were in CHEK2 (11%), ATM (9%), PALB2 (8%) and the genes associated with Lynch syndrome (7%).
Most respondents were white, female and cisgender. Only 10 men completed the survey. Over half of the respondents were over the age of 50 (57%). The full demographics can be viewed here.
Respondents needed genetic counseling and testing information and resources
We asked our respondents to share the information and resources they needed and used related to genetic counseling and testing. The largest gaps were between the need and use of the following:
- Information about managing early menopause
- Financial navigation
- Financial support
- Resources for sharing genetic information with children
- Resource navigation
- Peer support
Comments from respondents also highlighted gaps:
- I was not prepared for how I felt, knowing that I was high risk for getting cancer but not knowing when. I didn’t know this at the time, but I needed help processing the outcome of the testing.
- I still do not know about resources for sharing genetic testing with children and would be interested.
- I thought I would be kept informed by my genetic testing service and oncologist as more was learned about my mutation, putting me at significantly higher risk for breast cancer. (I had already been treated for advanced ovarian cancer.) But no one ever followed up with me. I learned about these new developments on my own years later, and I still need better direction on prevention, surveillance, screening and prognosis.
- I found FORCE shortly after I tested positive for BRCA2 mutation. So, I had a great amount of support back when I tested. Wish I knew about FORCE before I tested!
- Honestly, it felt like someone handed me a bomb and it was going off and I had to figure it out for myself. My least favorite sentence I heard so many times was ‘It’s out of the scope of my practice.’
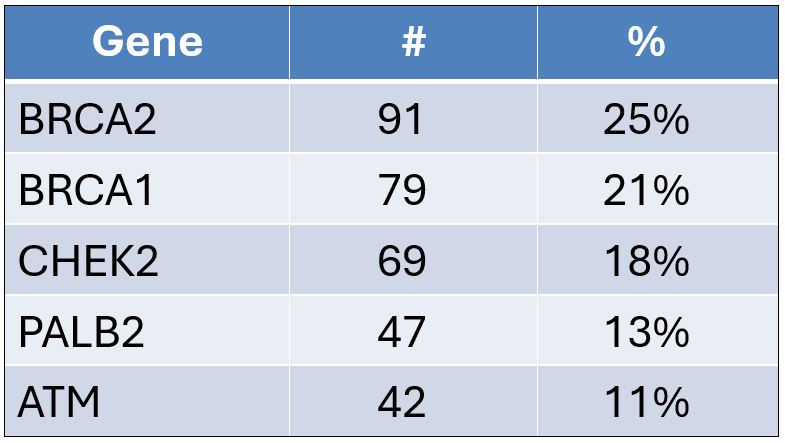
About 31 percent of respondents had been diagnosed with breast cancer. Among these, the most common genes represented were:
Breast screening for high-risk people
Screening for people at high risk for breast cancer typically includes:
- Clinical breast exams by a doctor.
- “Breast awareness,” which involves being aware of how your breasts should look and feel and report any changes to your doctor.
- Mammograms.
- Breast MRIs.
National guidelines recommend increased screening in people at high risk for breast cancer. The starting age, frequency and type of screening depends on the gene mutation. For some genes, such as BRCA1 and BRCA2, screening may start as early as age 25. National guidelines also outline screening for high-risk men with mutations in BRCA1, BRCA2 and PALB2. Visit our webpage on hereditary breast cancer screening for more information.
People faced barriers to high-risk screening
Most of the respondents at high risk for breast cancer indicated that a healthcare professional instructed them how to check their breasts for cancer (79%) and most (74%) reported that they examined their breasts regularly.
Nine percent of respondents said they took chemoprevention medication to lower their risk of breast cancer. Of these, 77% were previously diagnosed with breast cancer. Of the people who provided details about the medication they took, most indicated they took raloxifene or tamoxifen.
Of the high-risk women who had not been diagnosed with breast cancer and had not had double mastectomies:
- 89% receive regular mammograms.
- 75% receive regular breast MRIs.
- 92% receive regular clinical breast exams.
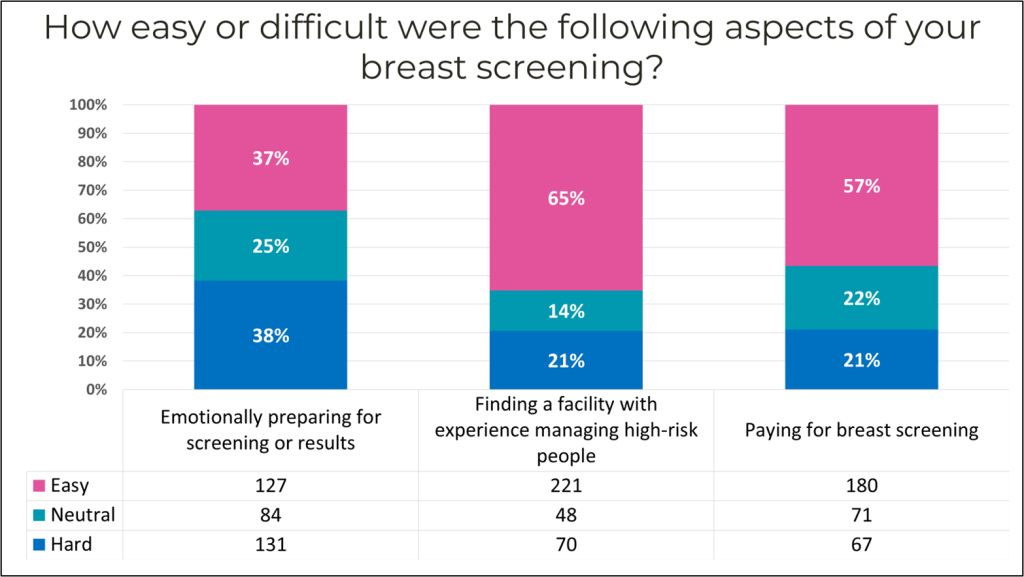
Our community faces barriers to undergoing guideline-recommended high-risk screening. When asked about these barriers:
- 38% said it was emotionally difficult preparing for screening or receiving results.
- 21% said it was difficult paying for breast cancer screening.
- 21% said it was difficult to find a facility with experience managing people at high risk for breast cancer.
Comments about high-risk screening
High-risk screening is costly
Although most people did not indicate they had difficulty paying for screening, most of the fill-in comments from respondents related to the high out-of-pocket costs for MRI screening:
- Medicare does not pay for any screening more frequently than annually, regardless of risk status, and there is no way to request exceptional authorization.
- Paying for the screening is a nightmare. I don’t get anxious about test results; I get anxious about dealing with my medical providers’ billing office.
- Last year, my insurance company denied paying for my breast MRI. I had it done anyway. I thought it was illegal to deny payment for this procedure because I have the BRAC2 gene mutation.
- Overall, getting the screening I need has been incredibly difficult, and I have achieved regular screening solely because I am determined and in charge of my healthcare management. I have called and written appeals for insurance/financial aid when I can’t afford it, informed doctors about screening needs repeatedly and insisted on screening when doctors didn’t follow guidelines.
- Even though I have fairly good insurance, I was surprised my mammograms were only partially covered. I ended up paying a couple hundred dollars for the screenings. I still haven't gotten my MRI and I'm nervous how much that's going to cost.
- Breast MRIs are expensive. Even with insurance, my deductible and co-payment leave me owing thousands of dollars. I have an MRI every other year due to this, even though my doctor recommends every year.
- The financial burden of MRIs and ultrasounds deters me from the additional screenings that are recommended.
- We changed insurance last year, and even though it says preventive care is 100% covered, they do not cover the breast MRI or the appointment with a high-risk breast surgeon.
High-risk screening causes anxiety
Many of our respondents expressed feeling anxious or fearful about their screening:
- This was more emotional than I thought it would be for the first several years.
- The waiting game was excruciating. I cried for two days and didn’t eat. I knew that having a double mastectomy was the ONLY thing that would bring me peace.
- It’s scary. My first mammogram after finding my mutations resulted in a biopsy. It was benign, but I get scared before every mammogram.
- Scanxiety is real.
- I was diagnosed with my mutation at 28. Now that I am in my 40s, I do find increased levels of stress associated with screenings, as I know my risk has increased significantly with age.
People need credible information
Respondents expressed a need for more information and knowledgeable healthcare professionals:
- I have had to advocate to have my needs for monitoring met. My provider was ordering regular annual screening mammograms until I sent her literature on recommended screening practices for people with BRCA1 mutations.
- The information always seems biased towards immediate removal of the body part versus other means of risk reduction. There is a significant paucity of helpful information for women during childbearing/breastfeeding.
- My daughter has a BRCA 2 mutation. Her doctors are telling her she will die if she doesn’t have double mastectomy and oophorectomy immediately. She is 33 and in good health.
Risk-management research
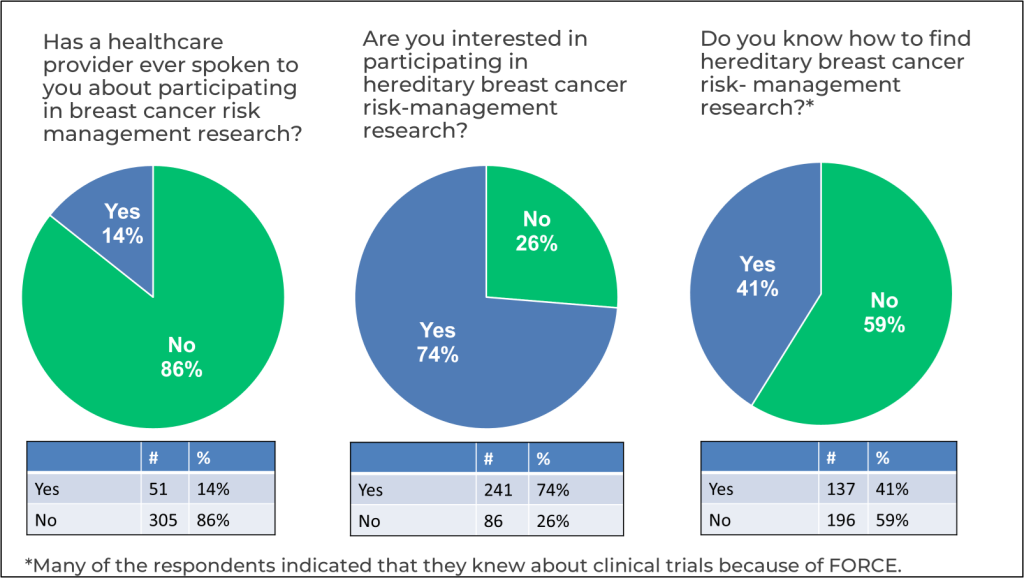
Research is the key to developing better breast cancer detection and prevention options. The hereditary cancer community is very motivated to participate in hereditary cancer research. Currently, studies are enrolling people at high risk for breast cancer. However, few of our high-risk respondents were told about available breast cancer detection or prevention research studies. Most were very interested in participating in such studies. We asked if respondents knew how to find breast cancer risk-management research studies; less than half knew how to find these studies. Of the respondents who did know, many identified FORCE as their source of research information.
Mastectomy for high-risk people
Of the high-risk respondents who never received a diagnosis of breast cancer, slightly more than half (52%) indicated that they had undergone a risk-reducing double mastectomy or were in the process of scheduling one.
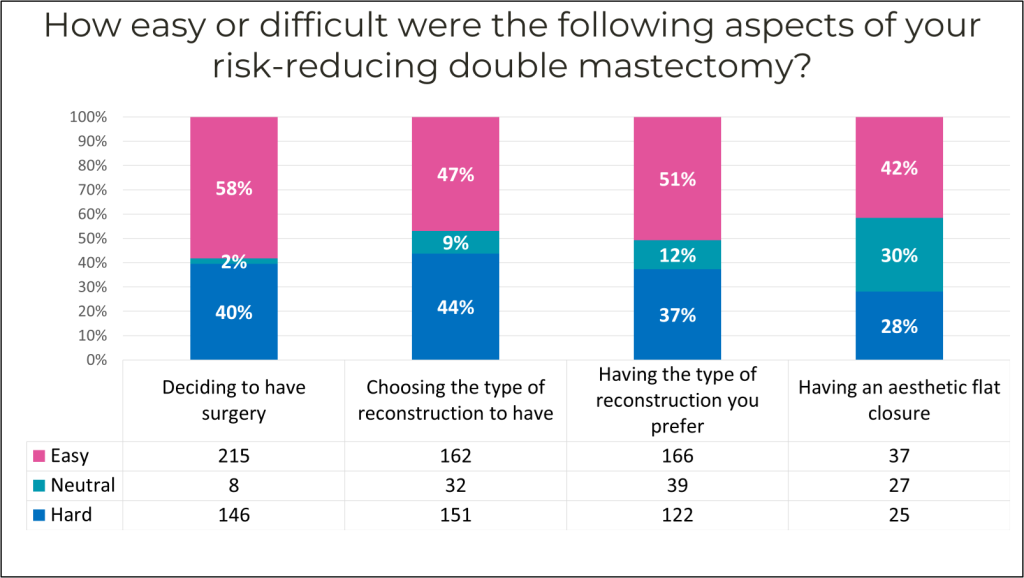
People faced barriers to risk-reducing double mastectomies
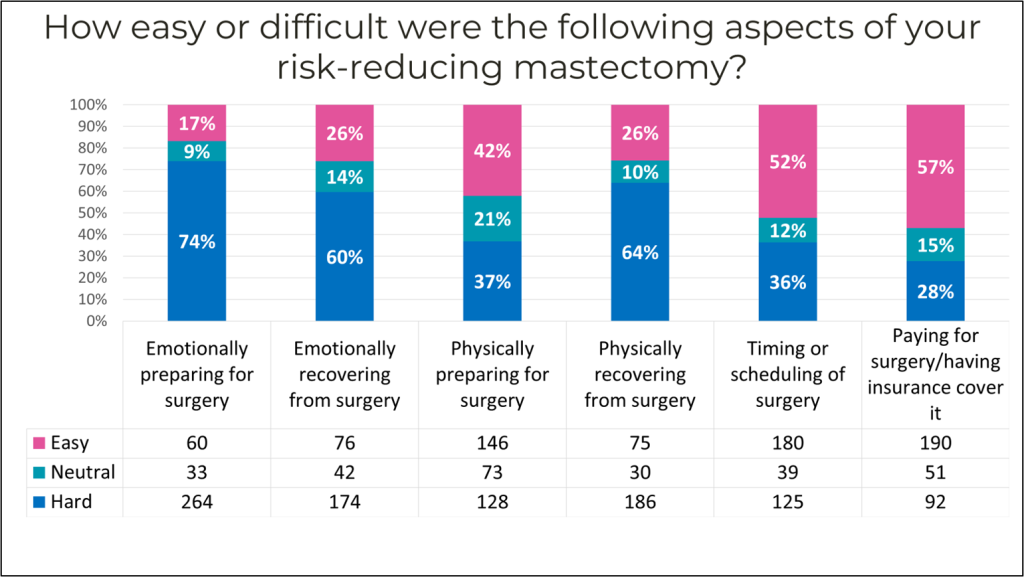
Many people in our community found the following aspects of mastectomy with or without reconstruction difficult.
- 40% had difficulty making the decision to have surgery.
- 44% had difficulty determining which type of surgery they should have.
- 37% had difficulty having the type of reconstruction they preferred.
- 28% had difficulty having an aesthetic flat closure.
Risk-reducing mastectomy takes a physical, emotional and financial toll on our community:
- 74% reported that emotionally preparing for surgery was difficult.
- 60% reported that emotionally recovering from surgery was difficult.
- 64% reported that physical recovery from surgery was difficult.
- 28% reported that paying for surgery was difficult.
Comments about emotional aspects
- I was not prepared for the emotion behind the feeling when I saw myself in the mirror for the first time and wondered who this new person is.
- The physical stuff is done, but the emotional recovery is still happening years later.
- I did a lot of research and talked to a lot of people prior to my surgery. I made a well-informed decision and do not regret the decision I made. I had lots of great support and medical care. But all of it was hard. No one ever wants to have to make this decision. I'm glad I had the surgery to reduce my risk of cancer.
- I was surprised at the level of relief I felt and how heavy the load of anxiety had been before surgery was done. Still, coming to terms with my new breasts was emotionally challenging (and still is sometimes).
Comments about physical recovery
- No one mentioned how long the nerve pain could last—and that there would be NO solution when in pain. After the simple mastectomy, I had an infection that caused problems I am still dealing with now.
- I’ve had multiple, extremely challenging complications from my reconstruction, and over five years and six surgeries later, I am still dealing with the repercussions (nor am I done with the reconstruction).
- There was a lot of information I wasn’t provided before about my surgery and recovery. It was a lot harder than I expected.
- I had a risk-reducing mastectomy with direct-to-implant reconstruction in 2015. Over time, the implants were uncomfortable and I learned of the risk of Breast Implant Associated Anaplastic Large Cell Lymphoma (BIA-ALCL).
Comments about the financial burden
- There is so much obfuscation around insurance fees and coverage. I planned one year ahead to select an insurance plan and ensure my surgeon would be in-network. Prior to my surgery, I worked for three months negotiating and confirming my surgeon would stay in-network and costs would be covered. Despite this, the morning I walked into surgery, I was asked to sign a form confirming I would pay $75,000 in medical fees. This, above all else, was the most daunting, scary, demoralizing aspect of my surgery.
- I was scheduled to have my surgery and reconstruction. My insurance denied coverage the night before my surgery. This was an emotional rollercoaster—mentally preparing for the surgery, then a crash of realization that it wasn't going to happen.
Comments about learning options and finding expert care
- I could have benefited from more education about the reconstruction options available. I was told one choice was it.
- I consulted with multiple surgeons who all gave different suggestions, so that was stressful to navigate. I also think surgeons should be more upfront about the loss of sensation in the breasts and the potential emotional toll that could take—the surgeons I spoke with treated it as an afterthought (if they even mentioned it at all).
- Making the decision was easy for me with such high risk. Understanding the process and finding doctors was very difficult and time consuming. It was never explained to me that each plastic surgeon only does a certain type of reconstruction.
- Very difficult to find and have to put together your own team of surgeon and plastic surgeon and deal with insurance, etc.; not much discussion regarding long-term quality of life issues postsurgery.
Hereditary cancer caregiver burden
For the hereditary cancer community, younger-onset risk, risk for multiple cancers, shared risk with relatives and the fact that cancer risk can be passed down through the generations create a disproportionate caregiver burden. When asked, 65% of respondents provided caregiving or support for a relative with cancer. Comments from respondents highlighted the generational trauma of hereditary cancer. Many people indicated that they provided caregiving support, sometimes from a very young age to multiple relatives. As one respondent shared, “I was 8-10 years old, taking care of my grandmother and taking turns with my siblings. I expect this is not uncommon and that children caring for relatives rarely get support.” Several people shared the challenge of caring for a relative while they themselves were undergoing cancer treatment or risk-reducing surgery.
- My sister and brother were dying from cancer when I was having surgery. It was a difficult time.
- A devastating experience losing my mom to cancer and a few months later losing my sister also to cancer. Most of it is a daze.
- As a 17-year-old, I handled every aspect of care ranging from medical appointments, side effects, medical emergencies, the house and the bills—while in high school. It would have been useful to know of resources that could have helped me, even if it was grocery shopping or getting meals. Somedays were so overwhelming.
- I provided care for my mother as she was dying of cancer when I was ending my own cancer treatment and learning about my BRCA2 options. Tough times.
How FORCE programs address these needs
For 25 years, FORCE has provided information and resources that benefit the hereditary cancer community. As one respondent shared, “I found FORCE shortly after I tested positive for BRCA2 mutation. So, I had a great amount of support back when I tested. Wish I knew about FORCE before I tested!”
Information on genes and risk
Our respondents expressed a need for credible information on cancer risks and risk-management options. FORCE’s information library lists the guidelines for cancer risks, risk management and treatment for 25 genes and seven types of cancer.
Information on mastectomy, reconstruction and going flat
Many respondents expressed hardship finding information about, choosing and gaining access to risk-reducing mastectomy with or without reconstruction. Our web pages on risk-reducing mastectomy and reconstruction or going flat and our post-mastectomy photo gallery provide expert-reviewed information to help people make informed decisions.
FORCE provides peer support and navigation
Our survey results emphasized the emotional toll that hereditary cancer takes on individuals and families. We provide numerous ways for our members to receive support and navigation to resources from trained volunteers and peers who have faced similar challenges.
- Peer Navigation Program
We match constituents to trained volunteers who share the same mutation and set of circumstances. Peer Navigators provide individualized support and resources. - Online Support Meetings
These moderated meetings allow people to share their experiences and challenges in a non-judgmental, supportive environment. We offer general support meetings and special meetings tailored to previvors, caregivers and people from the LGBTQ+ community. Select meetings are offered in Spanish and American Sign Language. - Message boards and closed Facebook group
Our moderated forums allow people to share and ask questions of the community 24 hours a day.
Connecting people to hereditary cancer research
From our survey, it’s clear that many people who are interested in and motivated to participate in hereditary breast cancer research are not informed by their healthcare team about studies enrolling people like them. For this reason, FORCE’s Research Search and Enroll Tool provides plain language listings of prevention and treatment studies enrolling people with inherited mutations.
Advocating for affordable screening and prevention
Many people expressed hardships in paying for guideline-recommended screening, including breast MRIs. FORCE’s public policy efforts include state legislative efforts to pass laws requiring health plans to cover the cost of guideline-recommended screenings. Visit our page listing which states have laws requiring health plans to pay for supplemental and high-risk screening. We provide sample letters to appeal insurance denials of guideline-recommended, high-risk screening and preventive services.
Next steps
Results from this survey reinforced the need for current FORCE efforts and highlighted key areas where more resources and programs are needed. Many people indicated they were not aware of FORCE resources and programs. We will increase our awareness efforts, including dedicated outreach to healthcare professionals.
Over the next two years, we plan to work closely with partners to understand and address the needs of groups that are under-represented by this survey, including diverse racial and ethnic populations, autistic individuals, transgender individuals and high-risk men.
We have collected data on people at high risk for gynecologic, pancreatic and colorectal cancers and will publish our results in the next few months.
Stay connected with FORCE as we continue to provide the hereditary cancer community with the necessary support, information, and resources.
POSTED IN: Genetic Testing , FORCE And FORCE Impact , Emotional Health And Well Being , Previvor
TAGS: Breast Cancer , BRCA1 , BRCA2 , PALB2 , CHEK2 , ATM
4 Comments
October 30, 2024
This data is very helpful in understanding this population and the needs of the individuals and families.
Mary-Frances Garber
Reply
November 5, 2024
Thank you, FORCE, for providing this extremely important and helpful information. It really provides context and puts things in perspective.
Brad Hertz
Reply
November 5, 2024
BRCA2 Hispanics. My younger sister and I had early stage breast cancer with bilateral mastectomies. She passed from lung adenocarcinoma after her breast cancer recurrence, also had/have follicular thyroid cancer. Our mother lost her mother and 4 of her siblings to BRCA2 related cancers. She survived, over a 26 year period, breast, colon, thyroid and breast cancers and lost to ovarian at 80. No one else ever lived long enough to have multiple cancers. Has lung and thyroid cancer been part of BRCA2?
Carmelita Ann Haltom
Reply
November 10, 2024
The overarching effect of uncertainty of insurance payment for preventative services is what stands out to me here. As a Lynch Syndrome survivor, I can relate to all of the comments about payment issues. It's a huge burden for those with recognized mutations. We need to be engaged with legislators to change this issue. Breast MRIs and colonoscopies bring enough angst without adding the fear of going broke before diagnosis.
Paige Van Pelt
Reply