Study: Risk of peritoneal cancer is low for people with an inherited BRCA mutation after surgery
Summary
The risk of peritoneal cancer is low in people with an inherited BRCA1 or BRCA2 mutation after risk-reducing ovary removal (oophorectomy). The risk was even lower when risk-reducing surgery was done at a young age and after 2005 when removal of the fallopian tubes was included in the procedure. The findings of this research support the theory that like ovarian cancer, peritoneal cancer begins in the fallopian tubes and reinforces the age recommendation for surgery. (Posted 1/23/25)
Printer Friendly Page Read the Original Article
RELEVANCE
Most relevant for: People with a BRCA1 or BRCA2 mutation who have had risk-reducing surgery to remove their ovaries.
It may also be relevant for:
- people with a genetic mutation linked to cancer risk
- previvors
Relevance: Medium-High


Strength of Science: Medium-High


Research Timeline: Post Approval


What is this study about?
Researchers wanted to understand the risk of peritoneal cancer among women with a or mutation who had preventive surgery that removed both ovaries ( oophorectomy).
What is peritoneal cancer?
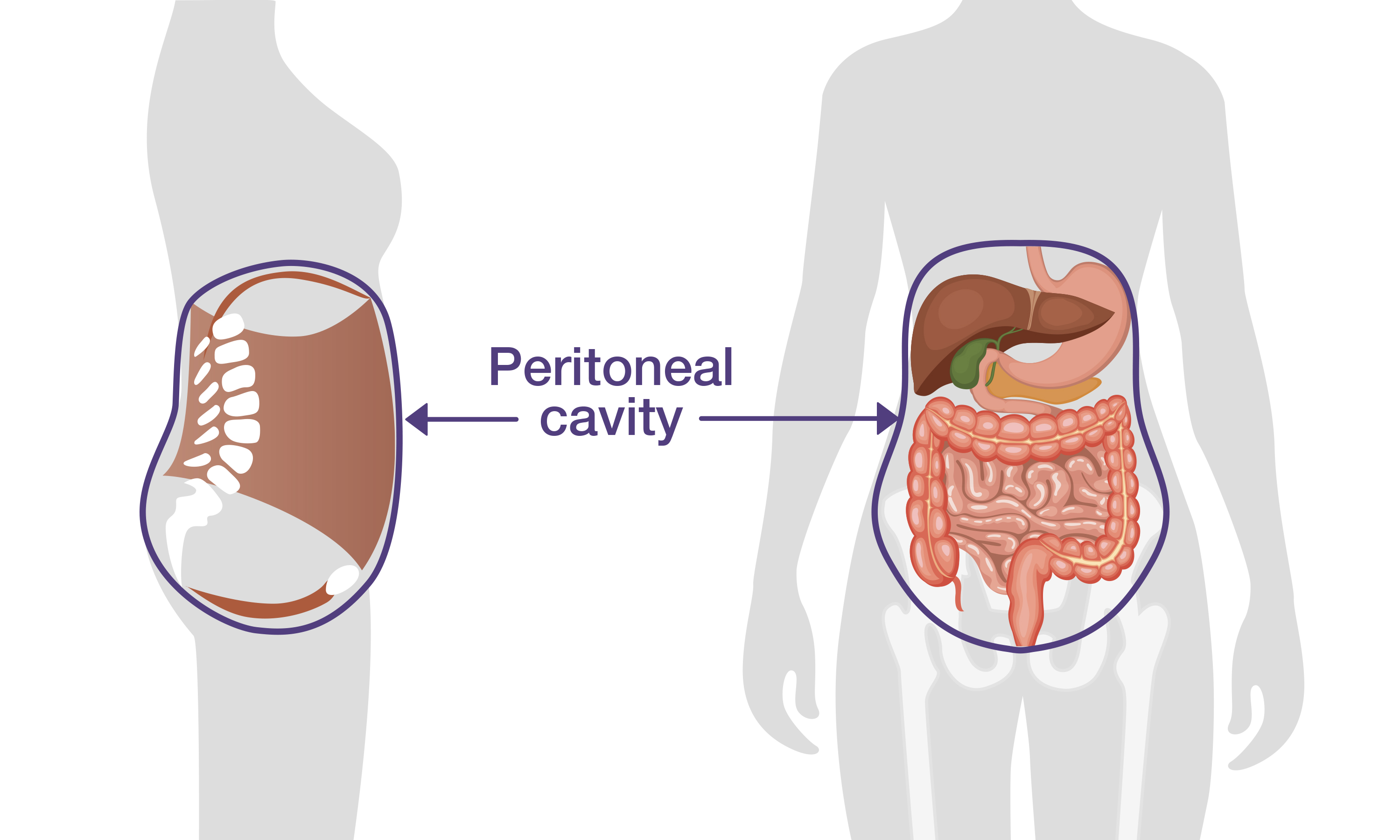
Peritoneal cancer is a rare cancer that looks and acts similarly to ovarian and cancer. It begins from the lining the cavity of the abdomen and covering the abdominal organs.
All three cancers (ovarian, and peritoneal):
- affect the reproductive system.
- look the same under a microscope.
- are treated similarly.
Due to these similarities, many professional medical organizations group peritoneal cancer with ovarian and cancers.
Risk factors for ovarian, fallopian and peritoneal cancers include a family history of breast and/or ovarian cancer and inheriting a mutation in a high-risk gene, such as or .
Why is this study important?
Until recently, experts believed that ovarian, and peritoneal cancers had separate origins. Now, however, they believe that most of these cancers begin in . Cancer or precancerous cells are thought to move from the to the ovaries and the lining of the abdomen (the peritoneum), resulting in ovarian and peritoneal cancer. For this reason, removing the () at the same time as risk-reducing removal of the ovaries () is now recommended for people with an inherited or mutation. This combined surgery is called risk-reducing salpingo-oophorectomy ().
Even after , some women develop peritoneal cancer. Researchers wanted to understand if these peritoneal cancers started in the lining of the abdomen or were caused by microscopic cancer cells that escaped into the abdomen before these women had surgery.
To better understand the risk of peritoneal cancer among women who have an in or and had risk-reducing removal of their ovaries, researchers studied how frequently peritoneal cancer occurred among this group. Studying mutation carriers who have had risk-reducing surgery will also give insight into where peritoneal cancer begins.
Study findings
This study included 6,310 women with a or mutation who had both ovaries removed ( oophorectomy). Women were monitored for almost eight years at 83 clinics in 12 countries.
During this time, 55 women developed peritoneal cancer:
- 45 had an in .
- 8 had an in .
- 2 had an in and .
Most people who developed peritoneal cancer after removal of both ovaries also had their removed:
- 48 had their removed at the time of their risk-reducing .
- 3 did not have their removed.
- It is not known whether the remaining 4 people who developed peritoneal cancer had their removed.
Risk of Peritoneal Cancer
Researchers were able to calculate the yearly risk of peritoneal cancer after risk-reducing surgery. The risk of peritoneal cancer was:
- 0.14 percent for mutation carriers.
- 0.06 percent for mutation carriers.
Researchers also calculated the risk of developing peritoneal cancer 20 years after risk-reducing surgery. The 20-year risk of peritoneal cancer was:
- 2.7 percent for mutation carriers.
- 0.9 percent for mutation carriers.
There were no peritoneal cancers in mutation carriers who had risk-reducing surgery before age 35. Similarly, there were no peritoneal cancers in mutation carriers who had risk-reducing surgery before age 45.
There was a sharp decrease in peritoneal cancers among women who had after 2005. An increased effort has been made henceforth to ensure that both ovaries and are removed at the time of risk-reducing surgery. This decrease in peritoneal cancer among mutation carriers supports the idea that peritoneal cancer, like ovarian cancer, begins in the .
What does this mean for me?
These results support the current recommendation that should be performed by age 35-40 for mutation carriers and before age 45 for mutation carriers. The remaining risk of peritoneal cancer after has been decreasing over the last 20 years and is now very small, likely due to inclusion of as part of standard of care for surgeries.
Reference
Narod SA, Gronwald J, Karlan B, et al. Incidence of peritoneal cancer after among and mutation carriers. Journal of the National Cancer Institute. 2024. 116(11):1753-1760.
Disclosure: FORCE receives funding from industry sponsors, including companies that manufacture cancer drugs, tests and devices. All XRAYS articles are written independently of any sponsor and are reviewed by members of our Scientific Advisory Board prior to publication to assure scientific integrity.
Share your thoughts on this XRAY review by taking our brief survey.
posted 1/23/25
The National Comprehensive Cancer Network (NCCN) provides guidelines for the management of gynecologic cancer risk in people with and mutations.
Prevention
- Risk-reducing removal of ovaries and , (known as risk-reducing salpingo-oophorectomy or ) is recommended between ages 35-40 for and 40-45 for and upon completion of childbearing.
- Research shows that removing the ovaries can increase survival for women with or mutations.
- Women should talk with their doctors about the effects of early menopause and options for managing them.
- Women should talk with their doctors about the risks and benefits of keeping or removing their uterus (hysterectomy), including:
- Women with a or mutation have an increased risk for a rare form of aggressive uterine cancer; hysterectomy removes this risk.
- For women considering hormone replacement after surgery, the presence or absence of a uterus can affect the choice of hormones used.
- Estrogen-only hormone replacement is less likely to increase the risk for breast cancer, although it increases the risk for uterine cancer. Women who still have their uterus are typically given hormone replacement with both and progesterone.
- Adding progesterone to hormone replacement can protect against uterine cancer. However, the combination of these hormones may increase the risk for breast cancer more than alone.
- A medical history of fibroids or other uterine or cervical issues may justify a hysterectomy.
- Oral contraceptives (birth control pills) have been shown to lower the risk for ovarian cancer in women with mutations. Research on the effect of oral contraceptives on breast cancer risk has been mixed. Women should discuss the benefits and risks of oral contraceptives for lowering ovarian cancer risk with their doctors.
- Removal of the only () is being studied as an option for lowering risk in high-risk women who are not ready to remove their ovaries. Studies on the effects of are ongoing. Whether lowers the risk for ovarian cancer in high-risk women remains unknown.
- Consider enrolling in a research study looking at this procedure to lower cancer risk.
Screening
- There are no proven benefits to routine ovarian cancer screening using transvaginal and a blood test. These tests are not currently recommended.
- After , a very small risk remains for a related cancer known as primary peritoneal cancer (PPC). There is no effective screening for PPC after
- Women should be aware of the symptoms of gynecologic cancer and report abnormalities to their doctors, particularly if they persist for several weeks and are a change from normal. These symptoms can include:
- pelvic or abdominal pain
- bloating or distended belly
- difficulty eating
- feeling full sooner than normal
- increased urination or pressure to urinate
Updated: 01/29/2025
The following resources can help you locate an expert near you.
Finding gynecologists with expertise in cancer risk and treatment
- The Foundation for Women's Cancer has a search tool to help you find a gynecologic oncologist.
Related experts
Some symptoms and conditions related to female reproduction may be managed by other experts.
Fertility experts
- The Oncofertility Consortium maintains a national database of healthcare providers with expertise in fertility preservation and treatment of people who are diagnosed with cancer or have a high risk for cancer due to an .
- Livestrong has a listing of 450 sites that offer fertility preservation options for people diagnosed with cancer.
Financial assistance may be available to make the cost of fertility preservation affordable for more patients. Patients are referred to those programs as needed.
Menopause experts
- The North American Menopause Society has a tool to help you find a qualified menopause expert in your area.
Sexual health experts
- The Sexual Medicine Society of North America (SMSNA) has a search tool to find experts in your area who provide sexual health care services.
- The American Association of Sexuality Educators, Counselors and Therapists (AASECT) maintains a tool to help people find a sexual health expert near them.
Other ways to find experts
- The National Cancer Institute (NCI)-designated comprehensive cancer centers deliver cutting-edge cancer care to patients in communities across the United States. Most centers have specialized screening and prevention centers for high-risk people. Find a center near you and learn about its specific research capabilities, programs, and initiatives.
- Register for the FORCE Message Boards to get referrals from other members. Once you register, you can post on the Find a Specialist board to connect with other people who share your situation.
Updated: 04/09/2023