Ovarian Cancer: Surgery to Reduce Risk
Surgery to Lower Ovarian Cancer Risk
Note that when we use the terms "female" and "women" we are referring to people assigned female at birth. This section covers the following topics:
What is risk-reducing salpingo-oophorectomy?
Risk-reducing salpingo-oophorectomy () refers to the removal of the healthy ovaries and to reduce a person's risk of developing cancer. Decades of research on in high-risk individuals has shown that:
- It is an effective way to lower the risk for ovarian and cancer. It does not completely eliminate the risk for these cancers. There is a remaining risk for primary peritoneal cancer even after the ovaries and tubes have been removed, but this risk is very small.
- It can lower the risk for death in high-risk women.
- It may also lower the risk for breast cancer in certain high-risk women.
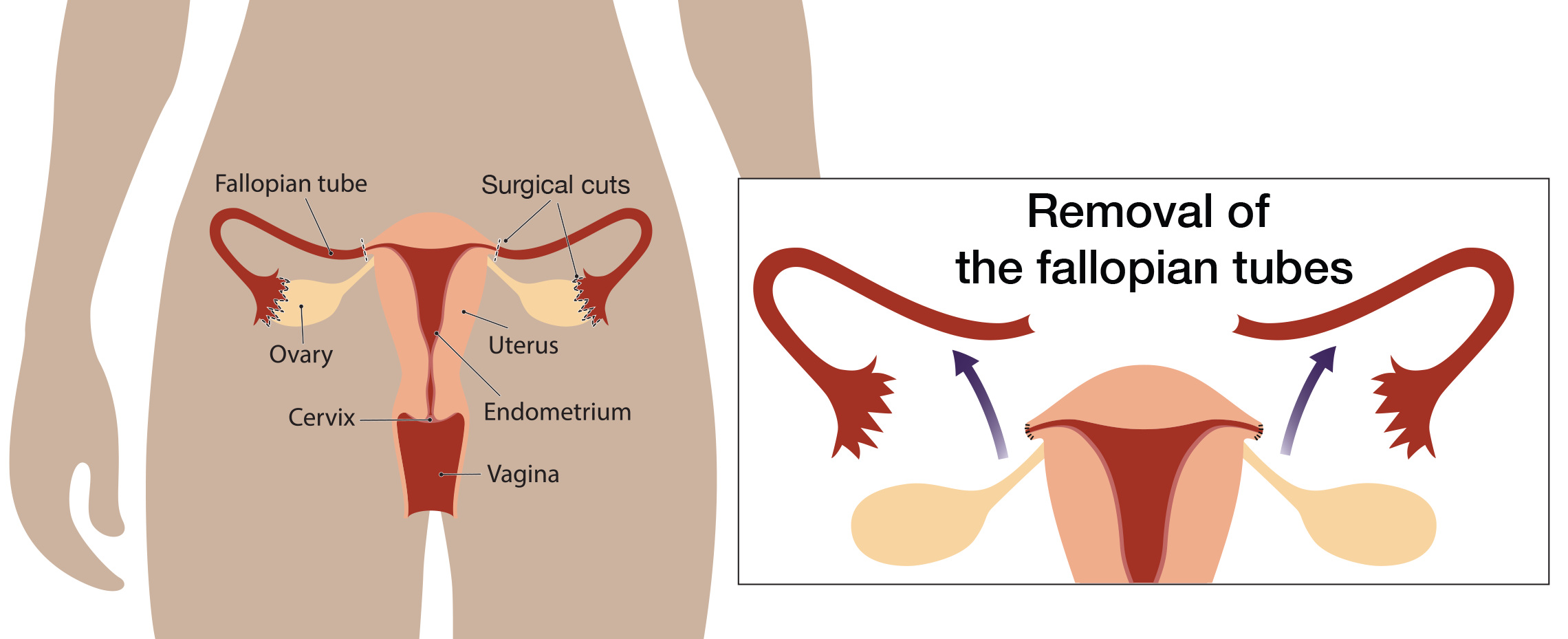
What is risk-reducing ?
involves removal of the only. Research suggests that the may be the source of many ovarian cancers. This has led researchers to study if it is safe to remove the only before menopause and delay removal of the ovaries until after menopause. Studies looking at to lower risk are currently enrolling people. Until these studies are completed, experts cannot say for certain that lowers the ovarian cancer risk in high-risk people. may be an option for high-risk women who are not ready to remove their ovaries. Experts recommend that women who decide to have surgery to remove their tubes alone have the completion as soon as they are ready.
Laparoscopic surgery
In the past, risk-reducing removal of the ovaries and tubes were performed using open surgery (also known as a laparotomy). This involves one long incision in the lower abdomen to remove the ovaries and , (and for those undergoing hysterectomy, the uterus). Today, risk-reducing removal of the ovaries and tube can usually be performed by laparascopic surgery. Laparoscopic surgery involves a small incision made in the abdomen to insert a flexible scope with a camera, which is used to see the ovaries and tubes. Addition small incisions are made to insert surgical instruments needed to remove the ovaries and tubes.
In general, people who have surgery by laparoscopy may heal quicker and spend a shorter time in the hospital than people who have open surgery.
Hysterectomy during risk-reducing salpingo-oophorectomy
Hysterectomy can be performed at the same time as , especially for people who have an increased risk for both ovarian and endometrial cancer. Mutations in some of the genes increase the risk for both cancers. Although the overall risk is not increased, some studies have shown that inherited mutations may increase the risk of a very rare but aggressive type of cancer called “uterine serous papillary carcinoma.” Medications like tamoxifen and progesterone may also increase the risk for uterine cancer.
People who have increased risk for ovarian cancer and average risk for endometrial cancer may still choose to remove their uterus at the same time that they undergo risk-reducing removal of their ovaries and . Factors that may affect the decision to remove or spare the uterus at the time of risk-reducing salpingo-oophorectomy include:
- Previous uterine or cervical abnormality:
Hysterectomy is often considered if a woman has had any previous abnormal pap smears or any abnormality of the uterus. - Considerations about hormone replacement:
Women who plan to take hormone replacement after may consider hysterectomy in order to simplify hormone replacement. There is an increased risk for uterine cancer in women who take alone compared to with progesterone. Women who have hysterectomy can take without progesterone. alone may have fewer side effects than with progesterone. See our section on Surgical Menopause for more information. - Intra-operative risk of hysterectomy:
Removing the uterus involves more surgery than alone. Therefore, there is a slight increase in operative complications and in the risk that a laparoscopic procedure will have to turn into an abdominal surgery with a full incision. - Insurance coverage:
Because of the surgery, recovery and hospitalization are lengthier; some insurance companies won’t pay for hysterectomy unless there is medical necessity. - Possible long term effects of hysterectomy:
Hysterectomy may increase the risk for some of the long term health issues which may be associated with .
Surgical risks and recovery
Every surgery has risks; some are more serious than others. Some risks can affect recovery or long term health
- Infection
- Delayed healing
- Blood loss
- Blood clots
- Pain (post-operative and long term pain syndromes)
- Surgical menopause and related health issues (see our section on Side Effects of Menopause for more information)
- Injury to internal organs
- Bladder incontinence
- Sexual side effects
It is important for people to discuss possible surgical risks with a surgeon to understand the seriousness and likelihood of these risks before making the decision to have risk-reducing surgery.
Average recovery time after is about 1-2 weeks. Recovery after open surgery is longer, up to 6 weeks.
Who should have risk-reducing removal of the ovaries and tubes?
The National Comprehensive Cancer Network (NCCN), is an organization of cancer experts that creates guidelines on cancer care and updates them yearly. NCCN's guidelines include recommendations for risk-reducing salpingo-oophorectomy based on an individual's gene mutation and situation. Each gene has a slightly different recommendation, click on the links for each gene for the full risk-management recommendation.
|
Gene |
Beginning Age |
Recommendation |
|
35-40 |
The guidelines recommend risk-reducing removal of ovaries and (). Timing of surgery should take into account plans to have children. is an option for people who are not ready to remove their ovaries. At this time, it is not known if is effective for lowering the ovarian cancer risk in high-risk people. People who choose should have a completion to lower their remaining risk for ovarian cancer when they are ready. |
|
|
40-45 |
||
|
45-50 |
The guidelines recommend risk-reducing removal of ovaries and (). Timing of surgery should take into account plans to have children. is an option for people who are not ready to remove their ovaries. At this time, it is not known if is effective for lowering the ovarian cancer risk in high-risk people. People who choose should have a completion to lower their remaining risk for ovarian cancer when they are ready. |
|
|
45-50 |
The guidelines state that people with mutations in should consider risk-reducing salpingo-oophorectomy. This involves having a conversation with your doctor to decide if the benefits of surgery outweigh the risks. The timing of surgery should take into account plans to have children. is an option for people who are not ready to remove their ovaries. At this time, it is not known if is effective for lowering the ovarian cancer risk in high-risk people. People who choose should have a completion to lower their remaining risk for ovarian cancer when they are ready. |
|
|
No set age |
More research is needed to determine whether people with mutations in benefit from risk-reducing surgery to remove their ovaries and . Currently, experts recommend that you have a discussion with your doctor about the benefits and risks of surgery taking into account your family history of gynecologic cancer. is an option for people who are not ready to remove their ovaries. At this time, it is not known if is effective for lowering the ovarian cancer risk in high-risk people. |
|
|
40 |
The guidelines state that people with mutations in these genes should consider risk-reducing salpingo-oophorectomy. This involves having a conversation with your doctor to decide if the benefits of surgery outweigh the risks. The timing of surgery should take into account plans to have children. is an option for people who are not ready to remove their ovaries. For people planning risk-reducing hysterectomy, the tubes should be removed at the same time. |
|
|
40 for at the time of hysterectomy 50 for salpingo-oophorectomy |
More research is needed to determine whether people with mutations in benefit from risk-reducing surgery to remove their ovaries. Currently, experts recommend that you have a discussion with your doctor about the benefits and risks of surgery taking into account your family history of gynecologic cancer. is an option for people who are not ready to remove their ovaries. For people planning risk-reducing hysterectomy, the tubes should be removed at the same time. |
|
|
50 |
More research is needed to determine whether people with mutations in benefit from risk-reducing surgery to remove their ovaries and . Currently, experts recommend that you have a discussion with your doctor about the benefits and risks of surgery taking into account your family history of gynecologic cancer. is an option for people who are not ready to remove their ovaries. For people planning risk-reducing hysterectomy, the tubes should be removed at the same time. |
|
|
Source: NCCN Guidelines: Genetic/Familial High-Risk Assessment: Breast, Ovarian, Pancreatic, , vs. 1 2026; Source: NCCN Guidelines: Genetic/Familial High-Risk Assessment: Colorectal, Endometrial, Gastric vs. 1 2025. |
||
Visit our Partners
Ovarian Cancer Research Alliance
Dedicated to fighting ovarian and all gynecologic cancers on all fronts while supporting patients and their families.
SHARE Cancer Support
Support and education resources in English and Spanish for people affected by ovarian cancer.
National Ovarian Cancer Coalition
Saving lives through the prevention and cure of ovarian cancer and by improving the quality of life for survivors and their caregivers.



